Parkinson’s treatment
When recommending a treatment, your doctor will take a number of factors into account, including your age and whether you have any other medical conditions. Your doctor will take your circumstances into consideration too, like the level of support you have from those around you and your ability to manage a treatment.
Bearing in mind that people respond in different ways to different treatments, the information here is intended only as a guide. You should discuss your options with your general practitioner, neurologist, movement disorder specialist or Parkinson’s nurse specialist, as well as your family.
Seven questions to ask your doctor about any new treatment:
- What are the treatment benefits?
- What are the potential risks?
- What is the cost of the treatment?
- Are there alternatives?
- What is the difference between treatments?
- Why do you recommend this treatment for me?
- What might happen if I do nothing?
Oral medications
Oral medications are often used to address the symptoms of Parkinson’s, such as tremors and movement difficulties. The four types commonly used are dopamine precursor medications, dopamine agonists, monoamine oxidase-B (MAO-B) inhibitors, and catechol-O-methyltransferase (COMT) inhibitors.
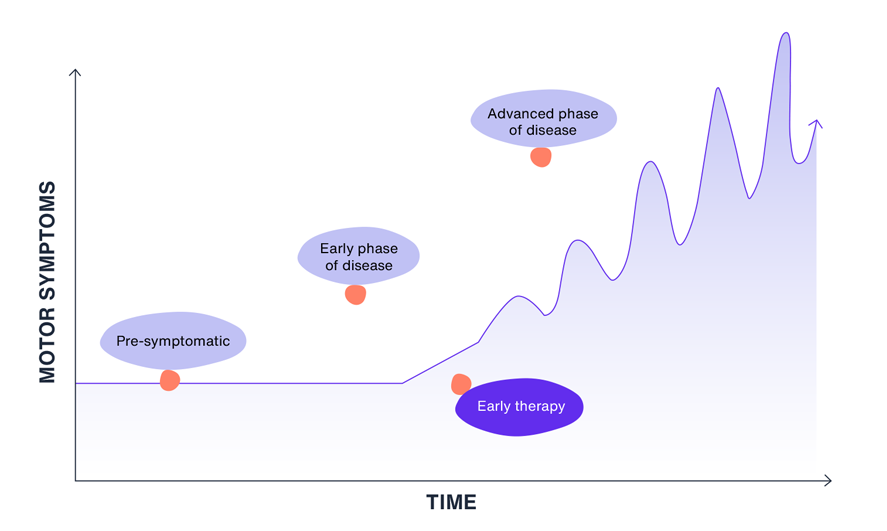
Over time you may experience your Parkinson’s symptoms progressing. Changes and additions may need to be made to your medication regimen to manage your symptoms. For example, you may find that you have to take a combination of tablets to treat your symptoms.
As Parkinson’s progresses it can change the way your body digests and absorbs food and medicine. As your symptoms progress the response to oral medication may fluctuate. Regular communication with your doctor about your experience with treatments and symptoms will help you and your doctor identify signs of progression and adjust management plans accordingly.
Sign of progressing Parkinson’s
If you are taking more oral medications more frequently, and experiencing an increase in symptoms, it may be a sign of progressing Parkinson’s. It may be beneficial to discuss any changes in your symptoms with your healthcare team and review your management plan together.
Non-oral therapies
When your symptoms become difficult to manage with oral medication despite changes to how often and how much you take, your healthcare professional may discuss other approaches, such as non-oral therapies, also known as device-assisted therapies.
Your health professional will advise if device-assisted therapies are suitable for you.
Pump therapy – under the skin

A continuous infusion can inject medication under the skin (subcutaneously). This requires a needle and infusion line to be fitted to an external pump, which you carry around with you.
Pump therapy – intestinal gel infusion

A type of medication that comes as a gel can be continuously pumped into your gut (small intestine) through a tube that is surgically inserted through your stomach wall. The pump is carried with you to enable a continuous infusion.
Neurosurgery (brain surgery)

Also known as deep brain stimulation - this procedure involves having very fine wires inserted into the brain to conduct electrical impulses to the affected nerve cells, similar to the way a pacemaker stimulates the heart.
If you feel that your symptoms are becoming unpredictable and hard to control, it may be time to discuss your Parkinson's management plan with your healthcare team.
Up until now, you have probably been taking your medication in tablet or capsule form. This is one of the most common modes of administration for Parkinson’s treatment.
While medications may help address symptoms for a period of time, the improvement is not permanent. Your doctor may have had to make repeated adjustments to your medications — adjusting the dosage and/or the number of times you take them or prescribing a combination of two or more medications.
As Parkinson’s progresses, the stomach’s ability to empty into your small intestine slows down which can cause bloating, feeling full too early, nausea, and in some cases constipation. This can impact the absorption of oral medications, leading to variable effectiveness in symptom control.
Symptom changes reflect the natural progression of Parkinson’s, not a measure of your past management or treatment success. If maintaining symptom control becomes more challenging, your doctor may discuss other management approaches with you. This can be an opportunity to adapt and explore new strategies to help you continue with your everyday activities.
Making treatment decisions
Moving to non-oral treatments can be a big decision that should be considered carefully in consultation with your specialist. Think about what’s most important for you and what you hope to achieve with your symptom management. To help you prepare for this discussion, take a look at these questions.
Having these discussions early with your specialist will help you to understand your options and consider what might be right for you now or in the future. Not all specialists are able to provide device-assisted therapies so you may need to be referred to another neurologist known as a movement disorder specialist.
Parkinson’s symptoms may impact your ability to make decisions in the future so advance care planning may be helpful.
- What are the treatment benefits?
- What are the potential risks?
- How do device-assisted treatments work and what symptoms might they address?
- What is the cost of the treatment?
- Are there alternatives?
- What is the difference between treatments?
- Why do you recommend this treatment for me?
- What might happen if I do nothing?
- Will I still be treated with oral therapies in conjunction with device-assisted treatments?
- What is the best timing to move to device-assisted treatments?
- Can I stop device-assisted treatments at any time?
- What complications are associated with device-assisted treatment?
- What support will I receive if I move to a device-assisted treatment?
- What will day-to-day management look like with device-assisted treatment?
- How will my lifestyle change?
- Will a device-assisted treatment mean I will be reliant on a carer?
- Will I be able to travel?
Caring for someone being treated with a device-assisted therapy
As Parkinson’s symptoms progress, loved ones may find themselves taking on carer responsibilities such as ensuring medication is taken on time, supporting mobility and providing emotional support. Therefore, any change to a treatment and management plan is often a decision made in partnership between those living with Parkinson’s and their families.
Moving to device-assisted therapy can change the type of care and support loved ones may provide.
It may be helpful to discuss any changes together so everyone involved understands what to expect.
Questions to ask a specialist, if device-assisted therapy is being considered:
- What are the implications or risks when moving to device-assisted therapies?
- How might my caring responsibilities change with device-assisted therapies?
- Will moving to device-assisted therapy affect my ability to work or participate in hobbies while providing care?
- Are there any specific resources or support services available to help me learn how to care for someone on a a device-assisted therapy?
If you notice a change in the symptoms of the person you are caring for, it is important to encourage them to speak with their specialist or healthcare team to discuss this and explore any additional management options that may be required.
Your healthcare team
As your symptoms progress it is important to ensure you are receiving appropriate advice and support tailored to your needs, so you can continue to manage your condition and maintain quality of life.
As your condition evolves, you may need to seek support from different healthcare professionals. If your general practitioner is your main point of contact, it may be worth seeking a referral to see a neurologist. If you are currently seeing a neurologist, they may refer you to a specialist neurologist, such as a movement disorder neurologist. They can help to further assess your condition if it’s advancing and recommend appropriate managment options should your condition require additional support.
There are other healthcare professionals who may play an important role in supporting you to manage your Parkinson's. For example, physiotherapists and occupational therapists can advise on how to maintain independence for personal activities and adjustments relating to your home. Speech pathologists can help support any speech or swallowing problems, psychologists can provide support for emotional or psychological problems and dietitians can advise on dietary needs to stay healthy.
Ask your general practitioner or specialist about how to connect with these healthcare professionals and services or programs that may be available to support you.
Exercise therapy
Exercise is important to maintain mobility, coordination and quality of life. It can also support mood and emotional health. Your GP or specialist may provide guidance on suitable activities or refer you to an exercise physiologist or physiotherapist who can help design a specific exercise program. To learn more about exercise therapy
visit the Fight Parkinson's Website
Keeping Healthy

There are some simple things you can do to help manage your Parkinson’s, such as staying active and focusing on your general health. This may include seeking advice from a speech pathologist or dietitian if relevant to your needs.
Staying Active

Staying both mentally and physically active can help to fight fatigue and maintain muscle strength and maximise movement.
Always speak with your healthcare professional before starting any new physical activity.
Lifestyle Tips

If your symptoms are changing, it’s a good idea to plan for changes in your lifestyle. One way is to remove clutter: having fewer obstacles in the house can simplify movement. Another idea is to avoid buttons as wearing clothes without buttons helps make dressing easier.
Making Changes Together

The support of the people around you is particularly important. Tell them how your symptoms may be progressing and let them know what changes you feel you need to make as a result.
Social Life

As your Parkinson’s changes, your relationships may change too. Keeping your friendships going, as well as looking to your partner, friends or family for support, can help you manage more easily.
Talking and Sharing

As your condition changes, you may find that you can avoid unpleasant or embarrassing situations by being open about your symptoms and explaining how you’re affected. This can help others understand what you are experiencing.
Frequently asked questions(FAQs)
For those having difficulty swallowing, avoid hard, dry, or crumbly foods or meat that is tough or chewy. Depending on your medication or treatment plan, there may be additional foods you need to avoid. Always follow the advice of your healthcare team.
Parkinson’s is usually a slowly progressive condition, but there are a number of things that can make your symptoms worse. These include stress, anxiety, poorly managed symptoms, lack of emotional support and reactions to some medicines.
Parkinson's is a chronic and complex condition, and a range of approaches may be used to help with symptoms. A healthcare professional is best placed to advise whether medication is appropriate for you.
Learn more about managing Parkinson’s
Parkinson’s management should always be tailored to each individual and their symptoms. Prepare for your future and learn more in our Advanced Parkinson’s guide – download your copy below.
AU-NEUP-250006. August 2025